trending topics
market reports
-
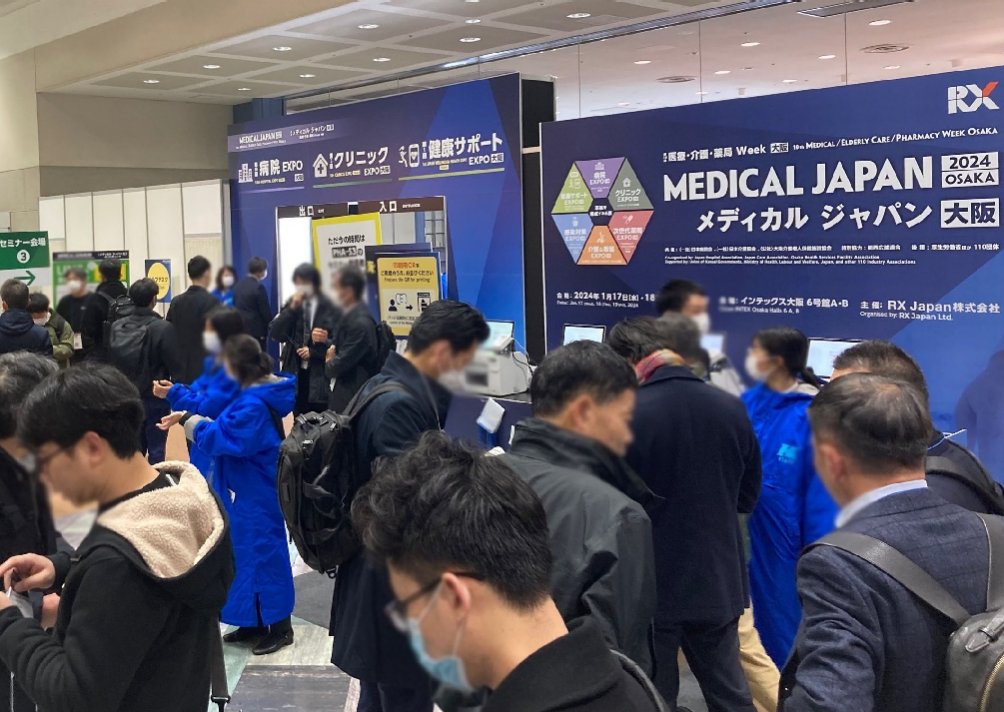
MEDICAL JAPAN 2025 OSAKA Returns to Showcase Global Innovations
2025-02-17
-

Visit MEDICAL JAPAN 2023 TOKYO and take full advantage of the business opportunities!
2023-09-01
-

US to distribute 400 million free N95 masks at CVS, Walgreens in COVID fight
2022-01-21
-

Ethiopia receives additional 2.2 mln doses of Chinese-donated COVID-19 vaccines
2022-01-21
-
Hong Kong researchers say they develop novel material able to kill COVID-19 virus
2022-01-14
-

10 million more Chinese doses on way for Kenya
2022-01-14
-

Sino-African ties on track for a brighter future
2022-01-07
-

Efforts urged to boost COVID-19 vaccine production capacity in poor countries
2022-01-07
-

UAE approves Sinopharm's new protein-based COVID-19 vaccine
2022-01-07
-

UAE approves Sinopharm's new protein-based COVID-19 vaccine
2022-01-07
Mask Up to Slow Down SARS-CoV-2
2020-10-23

This article is part of Harvard Medical School’s continuing coverage of medicine, biomedical research, medical education and policy related to the SARS-CoV-2 pandemic and the disease COVID-19.
Along with handwashing and physical distancing, the appropriate use of masks has stood as one of the essential pillars of infection prevention measures against COVID-19. However, rigorous evidence of masks’ effectiveness in blocking the transmission of SARS-CoV-2 has been limited. New research provides additional evidence of the benefits of universal masking in the health care setting.
The study, published in Occupational Medicine, found that universal masking in a Massachusetts health care system led to a flattening followed by a decrease in the COVID-19 epidemic curve among health care workers even as the infection rate continued to steeply rise in the surrounding community population.
Existing evidence of the efficacy of universal masking among health care workers is largely based on self-comparison results, such as comparing pre- and post-masking phases.
Researchers at Harvard Medical School and the Harvard T.H. Chan School of Public Health based at Cambridge Health Alliance conducted the study to explore the effect of universal masking in the health care system and used the statewide population as a comparison group.
Study senior author Stefanos Kales is HMS professor of medicine and division chief of occupational and environmental medicine at Cambridge Health Alliance.
The investigators compared the COVID-19 incidence rates between Cambridge Health Alliance health care workers and Massachusetts residents. The study period was from March 17, the date of the first COVID-19 positive incident in the health care system, through May 6, the date Massachusetts implemented public masking. Cambridge Health Alliance implemented universal masking on March 26, and peak COVID-19 incidence in Massachusetts was recorded on April 20.
The researchers categorized March 17 through 31 as the pre-intervention phase, allowing a five-day lag from the implementation of the masking policy to account for the average COVID-19 incubation period; April 1 to 20 the intervention phase; and April 21 through May 6 the epidemic decline phase. Temporal incidence trends were compared as the slopes of epidemic curves using seven-day averaged infection rates and compared using standardized coefficients from linear regression models.
The study showed that after implementing universal masking during the phase of rising infections in both the health care system and the community, health care worker infections sharply decreased, while community infections continued to rise until the state’s epidemic peak. Before the intervention, standardized infection rates showed almost identical increasing curves for the health care system and statewide population.
During the intervention phase, the health care system’s epidemic slope became negative, while Massachusetts’ slope remained positive. Once the epidemic peaked on April 20, both curves declined at similar rates.
“We found clear benefits to universal masking for preventing infectious spread within the work environment,” said Kales, who is also professor of environmental health at the Harvard Chan School. He added that “Our findings suggest that a universal masking policy should be implemented and maintained in health care settings as well as within indoor businesses when physical distancing and ventilation may be inadequate.”
Adapted from a Cambridge Health Alliance news release.



 My Member
My Member Message Center
Message Center